Epidemics in Aotearoa New Zealand
A DigitalNZ Story by National Library Services to Schools
This Topic Explorer set looks at epidemics in Aotearoa New Zealand and the Pacific over the last 200 or so years.
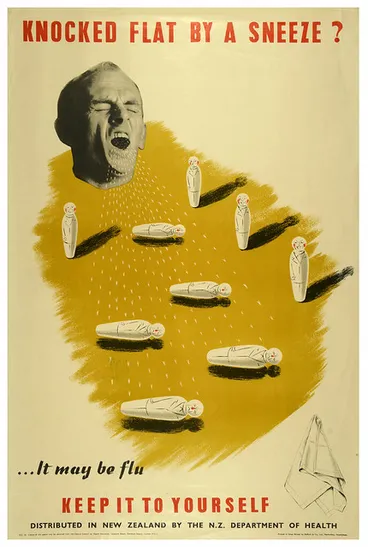
Knocked Flat by a Sneeze
Archives New Zealand Te Rua Mahara o te Kāwanatanga
BACKGROUND
This Topic Explorer set looks at epidemics in Aotearoa New Zealand and the Pacific over the last 200 or so years. Information on the 1918 Influenza epidemic and more recently Covid-19 can be found in the PANDEMICS AND EPIDEMICS.
EPIDEMICS: BACKGROUND
An epidemic is the abnormally high level of a disease at a particular time. It usually refers to infectious diseases, but it is also possible to have epidemics of non-infectious diseases such as heart disease and diabetes, and conditions such as obesity.
Source: Epidemics - Epidemics, pandemics and disease control, Te Ara - the Encyclopedia of New Zealand, (accessed 1 April 2020)
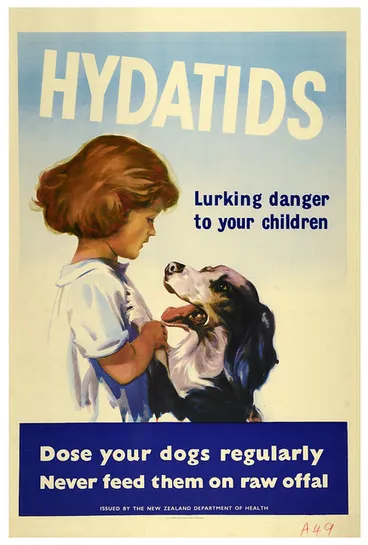
Hydatids Lurking Danger to Your Children
Archives New Zealand Te Rua Mahara o te Kāwanatanga
CONTENTS
This story on epidemics in Aotearoa New Zealand covers the following:
- Influenza
- Smallpox
- Measles
- Typhoid
- Tuberculosis
- Sanatoriums
- Polio
- Late 20th & early 21st-century epidemics
- Quick facts
- Department of Health posters
- Supporting resources
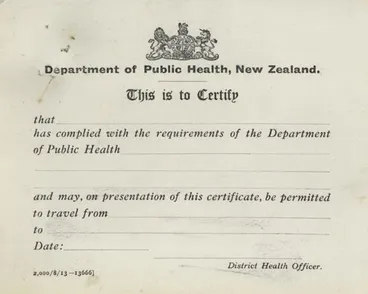
Smallpox vaccination certificate
Manatū Taonga, the Ministry for Culture and Heritage
INFLUENZA
European settlers brought new diseases to New Zealand in the early 19th century. Māori had little or no natural immunity to these diseases so suffered heavy mortality, particularly from measles and influenza.
INFLUENZA AND MAORI
Early influenza outbreaks among Māori were reported at Foveaux Strait in Southland between 1817 and 1820, and in the Bay of Islands and Mercury Bay in Coromandel in 1838 and 1839. In 1835 measles were reported among Māori working at the South Island whaling stations. T. A. Pybus wrote: ‘The death rate was serious, and in many cases the people died as they stood. Even in later years skeletons have been found far from their kaikas (settlements) … lying one across another indicating the suddenness of the end.’
Source: Epidemics - The typhoid era, 1810s to 1890s, Te Ara - the Encyclopedia of New Zealand, (accessed 6 April 2020)
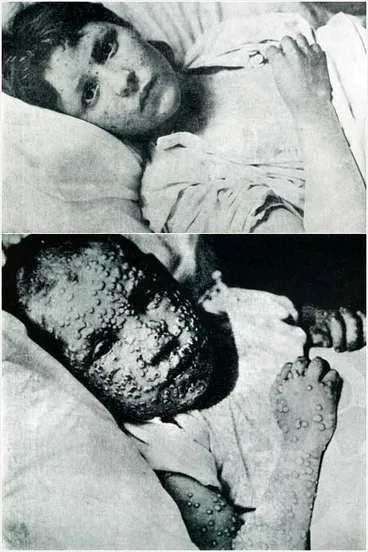
SMALLPOX
Smallpox is a highly infectious viral disease, which used to be a major killer worldwide before the discovery of effective vaccination in the late 18th century. Mass immunisation campaigns in the 19th and 20th centuries eventually eradicated smallpox – it now exists only in laboratory storage.
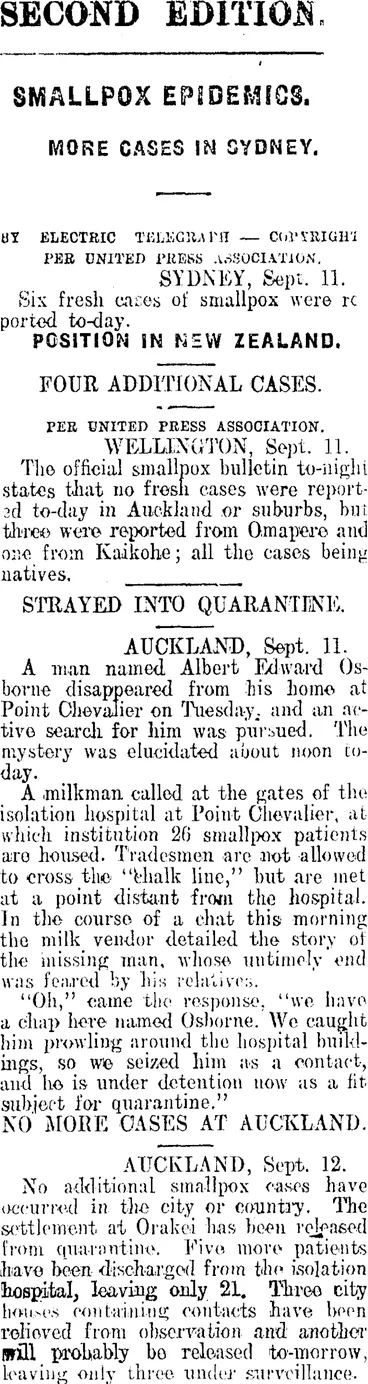
1913 NORTHLAND SMALLPOX EPIDEMIC
The most significant outbreak (of smallpox) occurred in 1913 in Northland. It was traced to a Mormon missionary who caught smallpox on a ship sailing to New Zealand from Canada. After he attended a hui in Northland in April 1913 the disease spread rapidly. Most of the 2,000 reported cases were Māori, as were the 55 who died.
A mass vaccination programme was set up and travel restrictions imposed to slow the spread of infection. Newspapers made much of the outbreak, blaming the epidemic on lack of sanitation and poor living conditions among Māori, yet Māori were much more willing to receive vaccination than many Pākehā.
Source: Epidemics - The influenza era, 1890s to 1920s, Te Ara - the Encyclopedia of New Zealand,(accessed 1 April 2020)
Smallpox
Manatū Taonga, the Ministry for Culture and Heritage
SECOND EDITION. SMALLPOX EPIDEMICS. (Mataura Ensign 12-9-1913)
National Library of New Zealand
EPIDEMIC. (Feilding Star, 20 September 1913)
National Library of New Zealand
Measles epidemic
Manatū Taonga, the Ministry for Culture and Heritage
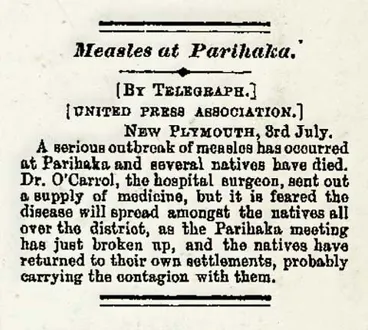
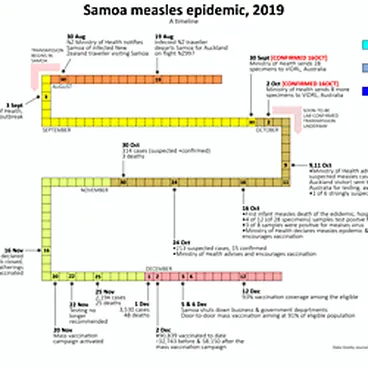
MEASLES
Measles is a very infectious airborne viral disease. Its symptoms can include, a rash, fever, sore eyes, coughing and a runny nose. Having measles can lead to other more serious complications often in children like, seizures, pneumonia and ear infections.
In 2019 there was a national outbreak of measles in New Zealand. From 1 January 2019 to 29 January 2020 there were 2193 confirmed cases of measles in New Zealand.
The epidemic also spread across the Pacific. Tragically, in Samoa, the measles death toll was (January 2020) 83. Many of the fatalities were children.
MEASLES VACCINATION
Luckily, protection from measles is achieved by vaccination. In New Zealand two doses of the MMR vaccine gives around 95% of the population full protection.
MMR stands for measles, mumps and rubella, these are three viral infections which can cause serious illness and quickly spread from one infected person though sneezing, coughing, or just talking.
Vaccination in New Zealand for MMR is available to all children from 12 months of age and also those adults, born after 1 January 1969.
If most people in New Zealand are vaccinated, MMR will not spread. This is known as herd immunity.
MEASLES. (Marlborough Express, 07 April 1911)
National Library of New Zealand
Measles: Health officials scramble as cases near 1000
Radio New Zealand
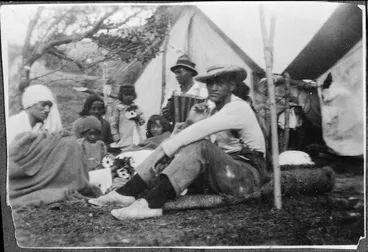
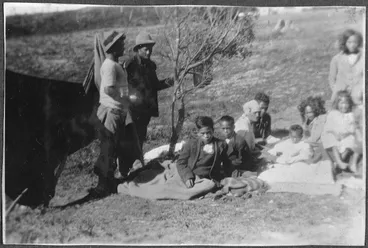
Typhoid camp, Maungapohatu
Alexander Turnbull Library
TYPHOID
Typhoid was one of the most common diseases of 19th-century New Zealand. It is transmitted by water, milk or food contaminated by the faeces of an infected person. It is caused by the bacterium Salmonella enterica typhi, which produces symptoms of high fever, sweating, diarrhoea, headache and cough.
TYPHOID IN AOTEAROA NEW ZEALAND
Early European settlements were often extremely unhealthy, lacking clean water supplies and effective sewage disposal. These created conditions favourable to the spread of infectious diseases. Typhoid and other bacterial infections were common, along with diphtheria, measles, whooping cough (pertussis), scarlet fever and tuberculosis.
Typhoid was especially prevalent in fast-growing towns or on the goldfields, where cesspits often leaked into water supplies. Infants and young children were especially vulnerable. Registered typhoid deaths in New Zealand peaked at 323 in 1875.
Typhoid death rates declined in towns and cities as sanitation improved, but persisted in rural and Māori districts well into the 20th century.
Source: Epidemics - The typhoid era, 1810s to 1890s, Te Ara - the Encyclopedia of New Zealand, (accessed 1 April 2020)
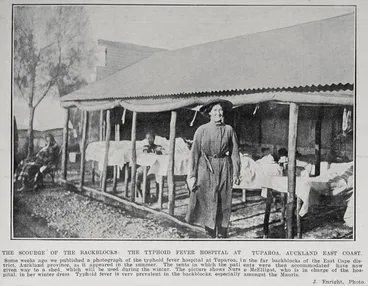
Typhoid camp, Maungapohatu, with Sister Annie Henry centre
Alexander Turnbull Library
Typhoid camp, Maungapōhatu, 1924
Manatū Taonga, the Ministry for Culture and Heritage
Typhoid camp, Maungapohatu
Alexander Turnbull Library
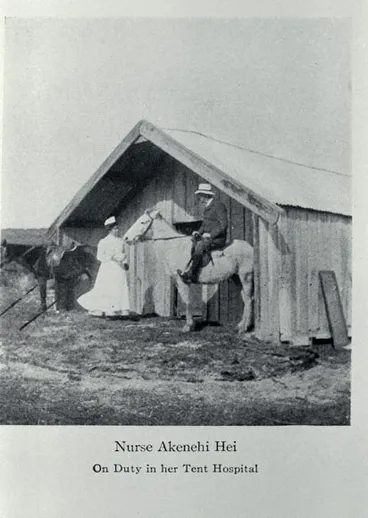
Nurse Ākenehi Hei
Manatū Taonga, the Ministry for Culture and Heritage
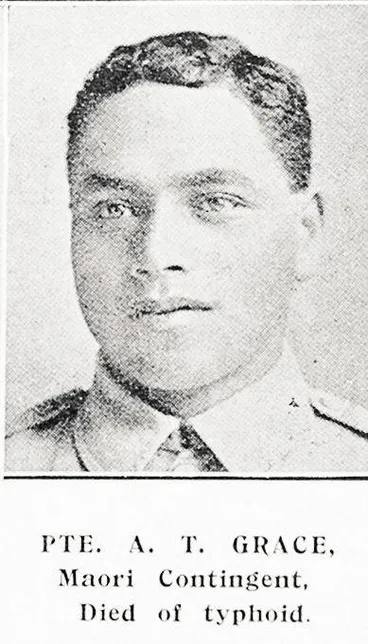
Private A. T. Grace, Māori Contingent, died of typhoid
Auckland Libraries
Frederick Ernest Smale
Manatū Taonga, the Ministry for Culture and Heritage
TUBERCULOSIS
In the late 19th century tuberculosis was a major killer of Pākehā New Zealanders, accounting for 10% of all deaths. Māori were even more vulnerable; by the 1930s their tuberculosis death rates were probably 10 times those of non-Māori.
In 1903 the Department of Public Health established Te Waikato, a sanatorium near Cambridge for the treatment of tuberculosis. It was open until 1922. Te Waikato provided open-air treatment, which consisted of fresh air, sunlight, exercise and good food.
Source: Hospitals - Spas, sanatoriums and surgery, Te Ara - the Encyclopedia of New Zealand, (accessed 8 April 2020)
After the Second World War a tuberculosis campaign began to bear fruit among Māori. From the early 1950s decreasing rates of tuberculosis incidence and mortality were recorded, particularly when Māori were immunised against it. In 1964 the Health Department stated that tuberculosis was no longer a significant cause of death among Māori.
Source: Te hauora Māori i mua – history of Māori health - Changing health, 1945 onwards, Te Ara - the Encyclopedia of New Zealand, (accessed 8 April 2020)
Fighting tuberculosis
Manatū Taonga, the Ministry for Culture and Heritage
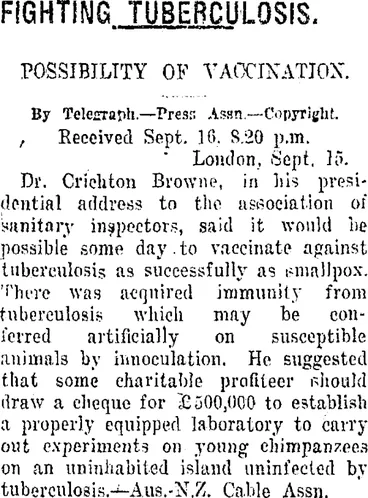
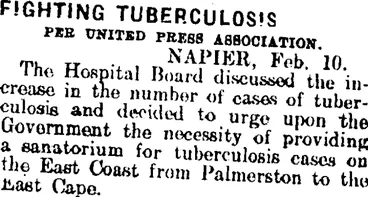
FIGHTING TUBERCULOSIS. (Taranaki Daily News 17-9-1920)
National Library of New Zealand
FIGHTING TUBERCULOSIS. (Mataura Ensign 10-2-1914)
National Library of New Zealand
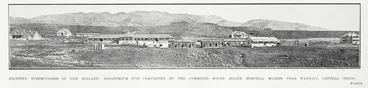
SANITORIUMS
By 1910 Wellington, North Canterbury and Otago all had sanatoriums. From 1908 Auckland Hospital Board provided accommodation for tuberculosis patients at the Costley Home (later Green Lane Hospital). Other hospitals also set up annexes to accommodate tuberculosis patients, and in the 1920s two further open-air sanatoriums were established in Hawke’s Bay and Otago. By the 1930s enthusiasm for this form of treatment waned in New Zealand (as elsewhere). It was replaced by surgery, albeit with little more success. Surgery was quickly abandoned once effective anti-tuberculosis drugs appeared (the first, streptomycin, was discovered in 1942). In the 1960s sanatoriums were closed or converted to other uses.
Source: Hospitals - Spas, sanatoriums and surgery, Te Ara - the Encyclopedia of New Zealand, (accessed 3 April 2020)
Ōkoroire sanatorium
Manatū Taonga, the Ministry for Culture and Heritage
Sanatorium, Waipukurau
MTG Hawke's Bay
The Sanatorium
Museum of New Zealand Te Papa Tongarewa
Otaki Sanatorium
Palmerston North City Library
Sanatorium - Rotorua
Alexander Turnbull Library
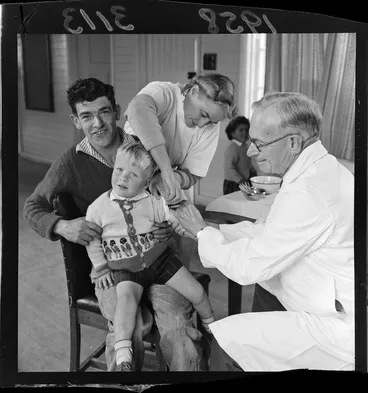
An unidentified child with his father getting a polio vaccination at Titahi Bay
Alexander Turnbull Library
POLIO
Poliomyelitis (polio), is an acute viral disease affecting the spinal cord and nervous system. Symptoms include fever, headache, malaise, pain and stiffness in back and neck, and partial or complete paralysis of limbs or the entire body. Case-fatality rates from paralytic polio have varied from 2% to 10%.
POLIO IN NEW ZEALAND
New Zealand experienced polio epidemics in 1916, 1925, 1927, 1937, 1948–49, 1952–53 and 1955–56.
Polio is typically a disease of children and adolescents, but the risk of paralysis increases markedly with the age of the patient, making young adults especially at risk if they catch this disease. In early outbreaks there was no effective treatment so careful nursing and palliative care (which alleviates symptoms rather than the cause) were the main medical responses.
The lives of seriously paralysed patients could only be saved by long periods in a compression chamber or ‘iron lung’. Survivors with a withered leg were fitted with strengthening callipers, which helped them walk. Public health campaigns in the 1950s stressed personal hygiene – schools provided buckets of disinfectant in their toilet blocks.
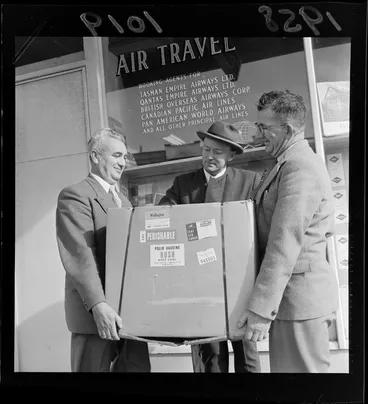
IMMUNISATION
Effective polio vaccines were developed in the 1950s. Jonas Salk’s inactivated vaccine of 1955 was followed by Albert Sabin’s weakened live virus oral vaccine in 1960. In New Zealand use of the Salk vaccine delayed the reappearance of polio between 1956 and 1961. After this a mass immunisation campaign using the Sabin oral vaccine achieved high population coverage and eliminated the polio virus from New Zealand.
Source: Epidemics - The polio era, 1920s to 1960s, Te Ara - the Encyclopedia of New Zealand, (accessed 1 April 2020)
Treating polio, 1943
Manatū Taonga, the Ministry for Culture and Heritage
Unidentified woman having a polio vaccination at Hotel Cecil, Thorndon, Wellington
Alexander Turnbull Library
Health Poster 'Careless Sneezing"
Archives New Zealand Te Rua Mahara o te Kāwanatanga
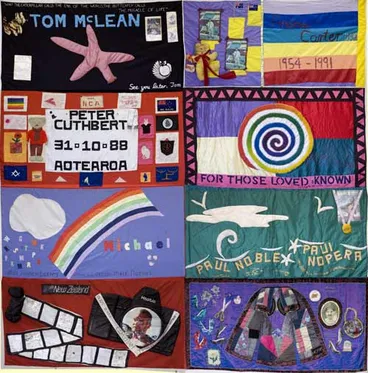
LATE 20th AND EARLY 21st-CENTURY EPIDEMICS
In 2009 there was widespread concern about the ‘swine flu’ pandemic. While there were 20 deaths in New Zealand, this was a tiny fraction of the 9,000 who died in the 1918 flu pandemic. Since the advent of vaccination, antibiotics and better sanitation, epidemics have been more readily controlled. The COVID-19 coronavirus outbreak in 2020 promised to be a severe test for the health system.
Source: Epidemics, Te Ara - the Encyclopedia of New Zealand, (accessed 8 April 2020)
THE IMPACT OF GLOBALISATION
Because of air travel, New Zealand is no longer an isolated country and has become affected by more diseases as they spread through the world; most notably HIV/AIDS, SARS (seasonal acute respiratory syndrome) and influenza. The 2009 influenza A (H1N1 – generally known as swine flu) pandemic caused more than 3,000 cases and 20 deaths in New Zealand.
Though epidemics have become less frequent, studies have found that hospital admission and discharge rates for infectious diseases have increased since at least the 1980s. This counters the prevailing wisdom that these diseases have become less of a burden. Despite improved uptake of annual influenza vaccination, seasonal influenza epidemics continue to have an impact, especially on older age groups. On average, approximately 40 deaths are linked to influenza each year.
The 2020 COVID-19 coronavirus pandemic was characterised by influenza-like symptoms and also affected older people disproportionately.
Source: Epidemics - New epidemics and new vaccines, 1970s to 21st century, Te Ara - the Encyclopedia of New Zealand, (accessed 1 April 2020)
AIDS memorial quilts
Manatū Taonga, the Ministry for Culture and Heritage
CUSTOMS. "I said SARS not SCARS." 1 April, 2003.
Alexander Turnbull Library
QUICK FACTS
- A 1903 NZ newspaper stated, ‘according to a reliable authority 80 per cent, of the children in the Colony under five years — the most susceptible age for becoming infected with smallpox — are not vaccinated.’
- There is a long history in New Zealand of people opposed to vaccination. As far back as 1884, the NZ Anti-vaccination Society had over 100 members.
- In the 1800s Māori were said to be very much in favour of smallpox vaccination after the 1849 publication of a pamphlet on smallpox written in Māori.
- Typhoid kills about 200,000 people globally each year, most in the developing world. However the last major outbreak of typhoid in NZ was in Auckland in 2017.
- By the end of 1913, 1777 Māori and 110 Europeans had been struck by an outbreak of the smallpox disease. Fifty five Māori died.
- In New Zealand, children receive their first MMR vaccination dose at 15 months. The second dose occurs at four years old. This is part of the National Childhood Immunisation Schedule.
- Between 1900 and 1911 twenty one cases of the plague were recorded in New Zealand.
- Famous New Zealand author, Katherine Mansfield died from tuberculosis in France. She was just 34.
- TB or tuberculosis was once called the Kings Evil. It was believed the kings of England and France could cure TB by simply touching people with the disease.
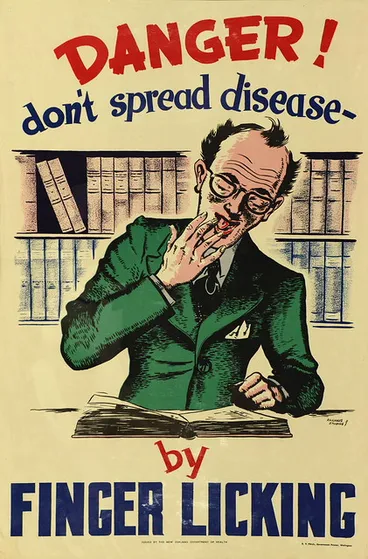
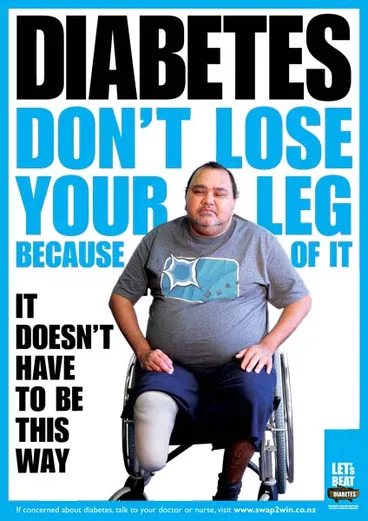
DEPARTMENT OF HEALTH POSTERS
The health-camp movement was founded on a belief that taking poor urban children to the countryside, exposing them to fresh air and sunshine, and feeding them well, would improve their overall health by making them stronger and less susceptible to diseases.
Source: Postage stamps - Stamps, 1855 to 1940, Te Ara - the Encyclopedia of New Zealand, (accessed 3 April 2020)
Over the years many other posters have been produced by the Government and New Zealand health organisations. They were and still are, used to warn the public or specific social groups about the dangers of potential diseases and also promote individual safe and healthy practices.
Health Poster 'Danger don't spread disease'
Archives New Zealand Te Rua Mahara o te Kāwanatanga
Diabetes poster
Manatū Taonga, the Ministry for Culture and Heritage
Immunisation Programme. Free [poster]
Puke Ariki
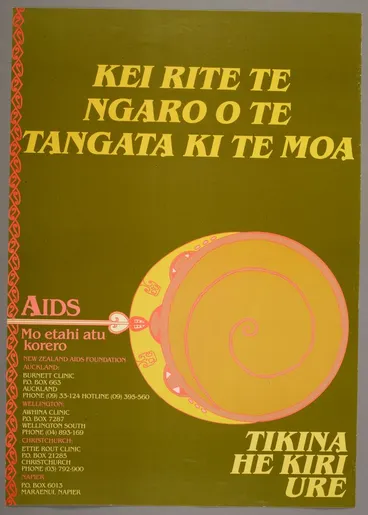
'Kei Rite Te Ngaro O Te Tangata Ki Te Moa' poster
Museum of New Zealand Te Papa Tongarewa
SUPPORTING RESOURCES
Animal epidemics — it's not just humans that have to deal with epidemics.
Chastising Its People With Scorpions — Māori and the 1913 smallpox epidemic.
Communicable Disease Control Manual — a list of communicable diseases, their symptoms and treatment from the New Zealand Ministry of Health.
Epidemics — This episode from the Aotearoa History Show goes into the history of epidemics in Aotearoa New Zealand including the impact of disease on Māori.
Lockdown lifted — what were the conditions of an epidemic lockdown like over a hundred years ago?
Measles stories — stories from parents who chose to delay or not get their children vaccinated against measles because of concerns about the measles, mumps and rubella (MMR) vaccine.
Polio — Nana Joy remembers the 1925 polio lockdown.
Polio epidemic — this page on Many Answers has links to reviewed websites and databases about New Zealand’s polio epidemic.
The plague — information about an outbreak of the plague in New Zealand and Australia in 1902.
Smallpox — a brief history of smallpox.
TB — a history of Tuberculosis (TB).
Te Wa o te Parekura (The Year of the Pestilence) — in 1913, 23-year-old Florence Harsant rode on horseback through the gumfields and isolated settlements of New Zealand’s far north and witnessed the 1913 smallpox epidemic.
The Smallpox Campaign — a detailed account of the Northland smallpox epidemic of 1913.
The truth about typhoid — Dr Mark Thomas explains what typhoid is and discusses whether the Auckland community is safe
Typhoid — Facts and speculation about Typhoid in 1889
Twenty of the worst epidemics and pandemics in history — plagues and epidemics have ravaged humanity throughout its existence, often changing the course of history.
Vaccination — an 1884 anti-vaccinator New Zealander writers a letter to the editor.
Vaccine — a 1929 account of how the smallpox vaccine is created using calves close to Wellington hospital.
Vaccines — how do they work and how have revolutionized modern medicine?
What is AIDS? — AIDS stands for Acquired Immune Deficiency Syndrome and is an advanced form of HIV. Not everyone that has HIV develops AIDS, largely thanks to advances in medications.
The Scourge Of The Backblocks
Auckland Libraries
This story was curated and compiled by Te Puna Mātauranga o Aotearoa | National Library of New Zealand, Services to Schools staff, March 2020.




![New Zealand. Department of Health: Consumption. A preventable disease - if treated early is curable. [Poster. 19]29. Image: New Zealand. Department of Health: Consumption. A preventable disease - if treated early is curable. [Poster. 19]29.](https://images.digitalnz.org/MQimO2AmG5urCyJzC8GHZGMSfP8=/368x0/https%3A%2F%2Fndhadeliver.natlib.govt.nz%2FNLNZStreamGate%2Fget%3Fdps_pid%3DIE77026)









![Give Health To Children. Buy Health Stamps for Children's health Camps [poster] Image: Give Health To Children. Buy Health Stamps for Children's health Camps [poster]](https://images.digitalnz.org/Q0xpkV7rWnpcAeWPD6Dy8xpYa5o=/368x0/https%3A%2F%2Fcollection.pukeariki.com%2Frecords%2Fimages%2Flarge%2F81533%2Fe3ec99670a12f31f65cc35c307bebed9ac9e2ccb.jpg)
![Immunisation Programme. Free [poster] Image: Immunisation Programme. Free [poster]](https://images.digitalnz.org/1_4ayCKi7muykL_hKYk2SLqV2Sw=/368x0/https%3A%2F%2Fcollection.pukeariki.com%2Frecords%2Fimages%2Flarge%2F81624%2F890ef9d79a8e2d51cb047a36c470c4479e11baf7.jpg)
![Coughs and Sneezes Spread Diseases. Trap the Germs in Your Handkerchief [poster] Image: Coughs and Sneezes Spread Diseases. Trap the Germs in Your Handkerchief [poster]](https://images.digitalnz.org/EqAhGvc9YodDn9r7_07oCFbie7k=/368x0/https%3A%2F%2Fcollection.pukeariki.com%2Frecords%2Fimages%2Flarge%2F81614%2Fd53e9e329657ed3a072dec12823df6ffd6971212.jpg)
![Don't Spit! It's Disgusting and Dangerous [poster] Image: Don't Spit! It's Disgusting and Dangerous [poster]](https://images.digitalnz.org/Ud88R1iRwP51xJpWX7OzUAX-k_w=/368x0/https%3A%2F%2Fcollection.pukeariki.com%2Frecords%2Fimages%2Flarge%2F81635%2F7a4898d95db9d3817f830ab16c93fadb060cebc0.jpg)